The big idea
By using a sewage-handling robot, our laboratory has been able to detect coronavirus in wastewater 30 times faster than nonautomated large-scale systems. This advance, published in the microbiology journal mSystems, provides even more lead time to communities monitoring their wastewater for early warning about local cases of COVID-19.
When clinical studies emerged showing that people who test positive for SARS-CoV-2 shed the virus in their stool, the sewer seemed like an obvious place to look for it. Wastewater surveillance can be used at the community level to see potential outbreak clusters before clinical diagnosis, especially in areas where COVID-19 prevalence rates far exceed testing rates.
The problem is that the virus is heavily diluted in the waste stream because of how many people’s bathrooms drain into it, not to mention all the other junk they flush. Surveillance depends on concentrating the viral particles from the wastewater to detect these low levels. This viral concentration step is typically the major bottleneck in wastewater analyses because it’s laborious and time-consuming. Our robot system takes a different, quicker approach.
Why it matters
Cities, schools and businesses around the country are using wastewater surveillance to find coronavirus in their midst.
Wastewater surveillance is especially useful as an early-alert system for high-risk areas, such as communities where undocumented residents may be cautious about individual testing.
The most commonly used viral concentration technique uses filters and can take anywhere from six to eight hours to transform a couple dozen sewage specimens into samples that can then be tested for the presence of SARS-CoV-2. Our new protocol concentrates 24 samples in a single 40-minute run.
We repurposed gear that usually performs microbiology or cell biology tasks in the lab to deal with sewage instead. By miniaturizing and automating our system, we eliminate a bunch of labor-intensive steps, resources and associated costs. And our hands-free process is much quicker.
How we do this work
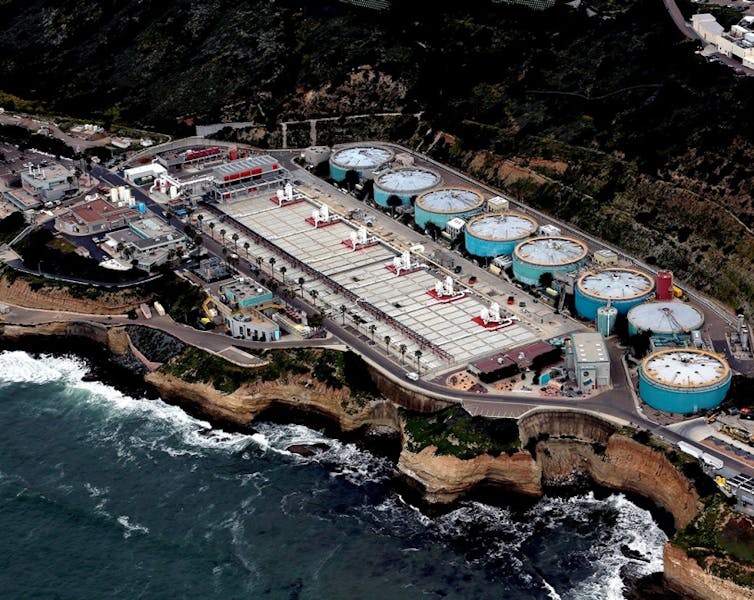
We gather sewage from autosamplers at San Diego’s main wastewater treatment plant, as well as from those we’ve deployed at over 100 manholes on the campus of the University of California, San Diego, which collect sewer samples every 30 minutes through the day.
Then, back in the lab, instead of relying on multiple filter steps, we use tiny magnetic beads to enrich the viral particles. We purchase these nanomagnetic beads that are designed to bind to a variety of respiratory viruses. The sewage-handling robot is equipped with a specialized magnetic head that snags the magnetic beads, with viruses attached. It preferentially fishes out viral particles, leaving behind the rest of the junk in the sewage sample.
Using a robot to automate the sewage concentration process lets us concentrate 24 samples in 40 minutes for each robot. Then the same robot can extract the viral RNA, processing 96 samples in 36 minutes. Finally, we use a polymerase chain reaction to search for the signature genes of SARS-CoV-2, much like a clinical diagnostic test that a lab would run on a patient’s nasal swab.
Overall, our system can process 96 samples in 4.5 hours, dramatically reducing the time from specimen to result.
What’s next
So far, ours is the only coronavirus wastewater study we’re aware of that uses an automated process.
We’re using this technique as a part of our large-scale wastewater surveillance on campus and sampling over 100 locations daily. San Diego school districts are also using it as an early-alert system.
We’re now using the viral genome sequencing part of our system to track the emergence of new SARS-CoV-2 variants.![]()
Smruthi Karthikeyan, Postdoctoral Research Associate in Pediatrics, University of California San Diego and Rob Knight, Professor of Pediatrics and Computer Science and Engineering, University of California San Diego
This article is republished from The Conversation under a Creative Commons license. Read the original article.